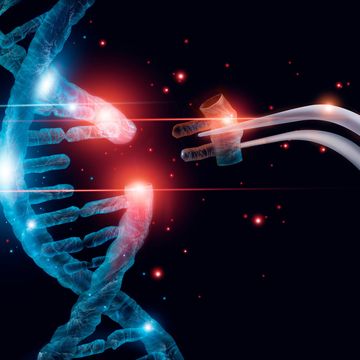
Magnetic Brain Stimulation
For the 20 percent of depressed patients who don't respond to drugs such as Prozac, the traditional last-ditch treatment option has been electroshock therapy. Recently, researchers worldwide began investigating a promising new alternative: transcranial magnetic stimulation. In TMS, magnetic pulses created by a metal coil attached to the scalp generate small electrical currents in the brain; these stimulate nerve cells in areas involved in depression--without harming surrounding gray matter. The treatment gained more momentum this spring when the Israeli firm Brainsway announced successful trials of its newest incarnation: deep TMS. "The magnetic fields of standard TMS devices extend only about half an inch into the brain's cortex," says Uzi Sofer, Brainsway's CEO. "But the coils of deep TMS can stimulate neurons farther inside the brain by projecting magnetic fields into the skull from several points around its periphery." This means that, for the first time, clinicians can target the brain's deep-seated limbic system, which plays an important role in mood regulation. So far, the device has lived up to its promise: 40 percent of the 64 depressed patients who received deep TMS achieved a clinically significant degree of recovery. As Brainsway lobbies for FDA approval of the device, Sofer is also evaluating deep TMS's suitability for Parkinson's and other neurological conditions that affect brain areas far below the surface.
Stem-Cell Scaffold
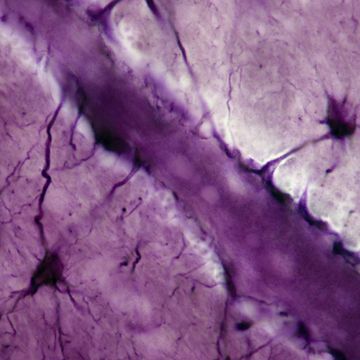
To pinch-hit for missing tissue at an injury site, stem cells need a scaffold to grow on--but artificial materials such as plastic won't do, since the body flags and rejects them as foreign substances. Ravi Kane, a biological engineer at the Rensselaer Polytechnic Institute in Troy, N.Y., has circumvented the problem with his biodegradable stem-cell framework made from alginate, a complex carbohydrate found naturally in brown seaweed. Time-release microscale beads called microspheres are embedded in the scaffold with a carb-eating enzyme called alginate lyase. As a result, the scaffold degrades at a tuneable rate once inside the body. Kane hopes the algal frameworks will allow doctors to implant stem cells directly into injured tissue--healthy bone stem cells at a fracture site, for instance, or neural stem cells in brain areas ravaged by Alzheimer's. Future versions of the scaffold could pack a one-two punch, delivering stem cells and drug compounds at the same time. "This is a modular system," Kane says. "There's still room in the scaffold to put other types of microspheres inside."
Instant Diagnosis
Since 1954, troopers have used breathalyzers to determine whether drivers have imbibed--and just how much. Jun Ye, a physicist at the University of Colorado, has transported the concept into an entirely new realm: medical diagnostics. The device he's designed detects thousands of different biological molecules in a single exhalation, creating a snapshot of the breath's contents that could signal the presence of illnesses, from cancer to cystic fibrosis. This split-second diagnosis is powered by a laser called an "optical frequency comb," which emits a wide spectrum of lightwaves that interacts with airborne compounds. "You have this rainbow of light coming out in a regularly spaced comb pattern," Ye says. "When breath molecules fly through the rainbow, they set off resonant frequencies that make the comb look like it has missing teeth." If the resulting pattern shows the presence of carbon monoxide, hydrogen peroxide and nitric oxide, for example, the exhaler may be suffering from asthma. "You don't have to wait days for test results," Ye says. "Within a minute, you know what's going on."
Pre-emptive Strike Against Cancer
Scientists around the world are working overtime on new cancer treatments, including more effective chemotherapy and better bone-marrow transplant procedures. Johns Hopkins biochemist Thomas Kensler aims to make all their efforts moot. Along with colleagues at Dartmouth College, Kensler is uncovering surprising ways to prevent malignancies from forming in the first place. Like an earthquake or avalanche, cancer is the end result of a whole sequence of unstable conditions: Abnormal cells must cluster in the wrong place at the wrong time, and cell-to-cell communications must break down, allowing cell proliferation and differentiation to proceed unchecked. Kensler has disrupted this sequence in the lab by treating healthy tissue with a chemical compound called CDDO-Im. Derived from acids in plants, CDDO-Im activates natural enzymes that remove toxic compounds from cells--compounds that might otherwise create DNA mutations that lead to cancer. CDDO-Im won't be available to patients for several years, but when it is, Kensler says, "I can see doctors recommending healthy people for this procedure based on their genetic susceptibility and the environmental conditions they've been exposed to. Our goal is to prevent that very first cancerous cell from tipping over the edge."
Implantable Nanowire
If Zhong Lin Wang has his way, routine blood-pressure checks at the doctor's office will soon be a thing of the past. The Georgia Institute of Technology physicist has designed an implantable nanowire that measures pressure fluctuations constantly, enabling patients to track their vital stats from home.
How does the sensor work?
The nanowire we use has two important properties: It's both a semiconductor and piezoelectric. That means that if there's an external mechanical force that bends the nanowire, such as blood vessel contractions, it creates an electrical field inside the wire. The presence of this electrical field affects the wire's conductivity, which is something we can measure. If the conductivity changes, that indicates blood pressure is changing.
How is this an improvement over previous techniques?
Older devices have a wrap around the arm that's really large. But this sensor can be implanted into an arm and monitored in real time. Patients wear a watch-type unit that records the data, so if something abnormal comes up, the watch sends an alert signal to them or their doctor right away.
Does it have any other potential applications?
Scientists often need to measure very tiny amounts of pressure in an automatic way. In gas lines hundreds of miles long, for example, sensors like this could help prevent potential explosions.
Superbug Zapper
Antivirals and antibiotics have long been the first line of defense against superbugs like HIV and staph--but they have some serious drawbacks. Antivirals can wreak havoc on the pancreas and liver, and antibiotics don't work against mounting drug-resistant strains. In response, Arizona State physicist K.T. Tsen has developed the ultimate multipurpose treatment tool: a superfast infrared laser that zaps bacteria and viruses without harming surrounding tissue. What makes Tsen's approach so novel is that his laser bumps off pathogens by mechanical means, not chemical or biological ones. "We use the laser to create large vibrations on the protein coat of the bacteria or virus, exciting it to such a high-energy state that the weak links on the capsid, or outer shell, break off," he says. Since mammalian cells don't have such a shell, this method destroys unwanted bugs while leaving patients' bodies unscathed. Large-scale clinical trials are still pending, Tsen says, but preliminary in vitro experiments indicate the laser effectively destroys the HIV virus. "Based on our progress so far, I'm very optimistic--the laser might be in hospitals within a couple of years."
Targeted Delivery
Pills may treat symptoms of the illness they're designed to fight, but when they're absorbed into the bloodstream indiscriminately they can also trigger debilitating side effects. Chemotherapy agents, for instance, cause nausea and hair loss, while antibiotics can trigger fatigue and shortness of breath. To help patients avoid side-effect doldrums, researchers at Philips's pharmaceutical division are developing the medical equivalent of a targeted missile-delivery system. Philips scientists place particles of drugs inside microscopic bubbles of fluorocarbon gas and then inject them into a patient's bloodstream. After the bubbles have reached the area flagged for treatment, a technician administers a high-energy ultrasound pulse. "When you hit a certain ultrasound resonance, the bubbles break, and that disperses the particles," says Christopher Hall, lead researcher on the project. Hall hopes doctors will someday be able to use bubble-encased drugs to treat prostate, breast and brain cancers, eliminating the grueling physical toll usually associated with such therapies. "Microbubbles let you give a dose in a more rational way," he says. "You can deliver a high concentration of the right drug to the spot where you want it."
Bloodstream Bot
Nowadays, procedures like removing tumors or Roto-Rootering plaque-filled arteries can require long hospital stints. But a mosquito-size robot developed by Oded Salomon, an engineer at Israel's Technion Institute, may be able to pull off these surgical feats without making large incisions--so recuperation is much faster. Taking a cue from '80s PC games like Laser Surgeon: The Microscopic Mission, Salomon's 1-mm-dia. bot, dubbed "ViRob," uses its barblike metal arms to grip the insides of veins and arteries and excise small amounts of tissue with built-in slicers. To operate most surgical probes, surgeons must grasp an external handle that protrudes from the body, but ViRob has no such limitations. After the bot is injected into a vein, operators can manipulate its speed and direction by tuning an external magnetic field to a variety of frequencies. "You don't need to control ViRob manually from outside, so you can access areas that otherwise can't be reached," Salomon says. "And doctors might even be able to perform operations remotely while a patient is at home." He predicts specialists will begin using the robot for procedures such as biopsies and blood vessel repairs within five years.
EKG Untethered
Wake up in the morning, stick a featherweight patch on your chest and tackle your day with the assurance that computers are keeping a constant eye on your ticker. That's the vision moti-vating scientists at the Netherlands' Holst Center, who are developing a next-gen EKG monitor that trumps competitors' in size and convenience. "With conventional EKG systems, you have an electrode patch that is connected to a rigid box in your jacket pocket," says Julien Penders, a program manager for the project. "We go one step further--the entire device can be worn on the surface of the body." The secret behind the monitor's ultracompact design is a chip that detects signals from the patch's electrodes and readies them for wireless transmission to a com-puter. In most EKG sys-tems, this data-processing step siphons lots of juice, but the team's smart chip is optimized for low power consumption, eliminating the need for bulky battery packs--and paving the way for its use as a preventive medicine. "The less intrusive the technology, the better," Penders says. "You can monitor your heart rate by simply patching a flexible EKG to your chest."
Nano Cancer Fighters
Sangeeta Bhatia can relate to the film Fantastic Voyage, in which scientists shrink a team of doctors and inject them (and their submarine) into a patient to perform treatments. As an MIT biological engineer, she gets to turn sci-fi into reality, developing nanoparticles programmed to make a beeline for cancer cells and release chemotherapy drugs nearby.
How did you get into developing microscopic disease-fighters?
At MIT, I did my Ph.D. on how to use microfabrication tools--which had previously been used for building semiconductor chips--for tissue engineering to restore liver function. Then I got more broadly interested in the idea that there were all these ways to make tiny body parts using nanotechnology that people had developed for making paints and computers and things.
And now you make nanoparticles that vanquish cancer cells. How are they better than plain old chemo?
The particles have substances on their surfaces that make them home in on the cancer--one type contains a peptide that binds to proteins found in a tumor's vessel linings. This represents a new frontier in that you're taking the toxic chemotherapy cargo directly to the tumor, so you don't get the side effects of delivering a poison throughout the entire body.
When will this treatment be available to patients? Things like this take anywhere from five to 10 years to get FDA approval. In the meantime, we're also developing materials that can track what tumors are doing--whether they're becoming more invasive or getting ready to metastasize. We'd like to treat the cancer before it spreads.