No risky surgery, no invasive implant, no painful rehabilitation and certainly not "no treatment at all." When we go to the doctor's office, what we want to hear is, "There's a pill for that." Over the past year, a series of medical breakthroughs have brought five such magic-bullet pills one step closer to reality, aimed at diseases such as osteoporosis and type 2 diabetes. Once they're developed, these pills won't be cure-alls: A pill that builds bone mass won't provide the heart and muscle benefits of exercise, for instance, and a calorie-burning pill is no replacement for a healthy diet. But these pills could provide a novel remedy for certain conditions that remain difficult to treat.
Osteoporosis
Exercise can strengthen the skeletons of people with osteoporosis, but their frail bones make physical activity difficult and often dangerous. While at Stanford University, biomedical engineer Chris Jacobs and his colleagues found that a particular enzyme called adenylyl cyclase 6 (AC6) turns on a cell's bone-building genes when the bone is loaded with weight. A pill that mimics the activity of AC6 in the body, Jacobs says, "could make the skeleton feel like it's being loaded at higher levels than it actually is." Taking that pill would allow osteoporosis sufferers to get the bone-building benefits of exercise without risking fractures or falls.
Type 2 Diabetes
A new drug studied by Abhay Satoskar, a microbiologist at Ohio State University, and his colleagues can control the symptoms of type 2 diabetes in mice when taken orally. The drug is a lab-made molecule that blocks the activity of macrophage migration inhibitory factor (MIF), a protein that's involved in high blood-sugar levels and inflammation—two primary symptoms of type 2 diabetes. When diabetic mice were given the drug, their blood sugar levels went down; when they stopped taking it, their blood sugar went back up. Satoskar hopes the drug will work to block MIF activity not only in mice, but in the millions of people with type 2 diabetes as well. "This is not a cure," Satoskar says, "but it's something that will allow you to maintain normal blood glucose and control your symptoms."
Jet Lag and Insomnia
Jet-lagged travelers and insomniacs, rejoice: Researchers have finally decoded the signal that our body clock uses to keep time. For years, scientists thought that neurons in the brain's suprachiasmatic nuclei, or SCN, regulated our body clocks by firing a lot during the day and less at night. But University of Michigan mathematician Daniel Forger and his collaborators have found that only half the neurons in the SCN keep time, and they've decoded the much more complicated pattern of firing these neurons use to do so. "Understanding that signal is going to be very important for helping us figure out how to change it when it's not correct," Forger says. A pill that could reset our daily clock wouldn't only help people wrestling with jet lag or sleep disorders, he adds; an out-of-sync body clock is suspected to play a role in medical problems ranging from cancer to Alzheimer's to heart disease.
Weight Loss
When we think of fat, it's usually as something that makes our waistbands tighter. But medical research groups in Scandinavia, the Netherlands and the United States have discovered that a particular type of fat, known as brown fat, can actually help us slim down. Brown fat burns calories, converting them to heat rather than storing them as flab. A pill that can boost the activity of brown fat could help obese people, or others looking to shed pounds by burning more calories. It wouldn't be a quick fix, but a pill that increased metabolism by 500 calories a day would speed weight loss by a pound a week.
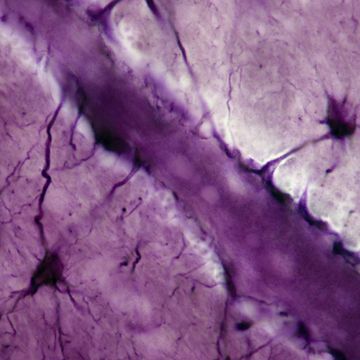
Male Contraception
A team led by reproductive-health researcher Michelle Welsh at the Queen's Medical Research Institute in Edinburgh, Scotland, has uncovered how a group of hormones called androgens—which include testosterone—control sperm production. The researchers looked at sperm production in two groups of mice. One group was missing the gene for androgen receptors (which the hormones can bind to) on certain testicular cells called peritubular myoid cells, while the other group had the gene. Mice with no androgen receptor produced much less sperm than the other mice. This new understanding of how hormones affect sperm production could eventually lead to a birth-control drug for men—the long-awaited male equivalent of the pill that revolutionized female contraception in the 1960s.