HER3-Targeting Antibody-Drug Conjugate Shows Encouraging Activity in Advanced Breast Cancer
U3-1402, an investigational antibody-drug conjugate targeting HER3, induced objective response in more than 40% of heavily pretreated patients with HER3-expressing breast cancer.
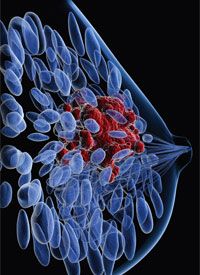
breast cancer
U3-1402, an investigational antibody-drug conjugate (ADC) targeting HER3, induced objective response in more than 40% of heavily pretreated patients with HER3-expressing breast cancer, according to results presented at the San Antonio Breast Cancer Symposium.1
The objective response rate (ORR) was 42.9% (18/42), including 40% of patients treated at the 4 mg/kg dose and 60% of those treated at the 6.4 mg/kg dose. The median progression-free survival (PFS) was 8.3 months months (range, 1.2-15.8).
The overall disease control rate (DCR) was 90.5% (38/42). DCR was 86.7% at the 4 mg/kg dose and 100% at the 6.4 mg/kg dose.
The median time to response (TTR) was 2.6 months (range 1.4-2.8). Most responses proved to be durable, as the median duration of response (DOR) was not reached (range, 2.8-13.8 months) after a median follow-up of 10.5 months. Twenty-one patients remained on treatment as of the November 6 data cutoff.
In preliminary results from 21 patients presented at the 2018 ASCO Annual Meeting, the ORR was 33% and DCR was 95%.2 “These results offer preliminary evidence of U3-1402 activity in HER3-positive metastatic breast cancer and further study is warranted,” lead author Norikazu Masuda, MD, PhD, National Hospital Organization, Osaka National Hospital, Osaka, Japan, said in a release. “The initial efficacy and safety data suggest that a HER3-targeting agent such as U3-1402 could provide a new treatment approach for patients with HER3-expressing metastatic breast cancer, who are in need of additional options to manage their disease.”
HER3 is overexpressed in breast cancer and several other types of tumors. U3-1402 consists of a fully human anti-HER3 antibody linked to a topoisomerase I inhibitor. To date, no HER3-targeted therapies have been approved.
Masuda and colleagues reported findings from an ongoing phase I/II trial (NCT02980341) to evaluate the safety, tolerability, and efficacy of U3-1402 in patients with HER3-overexpressiong metastatic breast cancer. The study comprises dose-escalation, dose-finding, and dose-expansion components.
Across the dose escalation and dose finding phases, 15 patients reeived the 4.8 mg/kg dose and 15 received the 6.4 mg/kg dose. The maximum tolerated dose was not reached during the dose-escalation part of the trial, and evaluation of those 2 doses continued in the dose finding part of the study.
The SABCS report represented an update of safety/tolerability and efficacy results. Investigator-assessed efficacy assessments included PFS, ORR, DCR, ORR, DCR, DOR, and TTR.
The data analysis included 42 patients who had a median age of 54.5 years. The cohort included 7 patients with HER2+ breast cancer, 21 with HR+/HER2- disease, 10 with triple-negative disease, and 4 with unknown molecular profile. The patients had received a median of 6 (range, 2-13) prior regimens, and 5 (range, 1-12) prior regimens for locally advanced/metastatic disease. More than 70% of the patients had liver and/or lung metastases, and 14.3% had brain/CNS metastases.
U3-1402 was generally well tolerated. Only 1 patient discontinued treatment because of treatment-emergent adverse events (TEAEs), and no fatal TEAEs occurred.
The safety analysis showed that 8 (19.0%) patients had TEAs requiring dose reduction, and 19 (45.2%) had TEAEs requiring dose interruption, most often neutropenia (23.8%), leukopenia (11.9%), and anemia and elevated liver AST (7.1% each).
Pulmonary AEs of special interest included 1 case each of grade 2 pneumonitis, grade 2 interstitial lung disease, grade 1 radiation fibrosis, and grade 3 radiation pneumonitis. The one patient who discontinued treatment because TEAEs did so because of grade 2 pneumonitis.
The most common (≥20%) all-grade AEs were nausea (85.7%), thrombocytopenia (71.4%), decreased appetite (66.7%), neutropenia (64.3%), leukopenia (59.5%), vomiting (54.8%), elevated liver enzymes (AST, 47.6%; ALT, 45.2%), anemia (38.1%), stomatitis (35.7%), diarrhea (31.0%), alopecia and fatigue (28.6% each), constipation (23.8%), and nasopharyngitis and malaise (21.4% each).
The most common (≥10%) grade ≥3 adverse events were thrombocytopenia (35.7%), neutropenia (28.6%), leukopenia (21.4%), anemia (16.7%), and elevated ALT (11.9%).
References
- Masuda N, Yonemori K, Takahashi S, et al. Single agent activity of U3-1402, a HER3-targeting antibody-drug conjugate, in HER3-overexpressing metastatic breast cancer: Updated results of a phase 1/2 trial. In: Proceedings from the 2018 San Antonio Breast Cancer Symposium; December 4-8, 2018; San Antonio, Texas. Abstract #PD1-03.
- Kogawa T, Yonemori K, Masuda N, et al. Single agent activity of U3-1402, a HER3-targeting antibody-drug conjugate, in breast cancer patients: Phase 1 dose escalation study. J Clin Oncol. 36, 2018 (suppl; abstr 2512).



