Design Strategies For Next-Generation Biocontainment Units
As the current COVID-19 pandemic continues to impact countries around the globe and concerns regarding the safety of the healthcare workers on the frontlines are growing, healthcare facilities are working hard to best support, manage, and protect patient-facing healthcare workers as they provide patient care.
This is driving a new discussion on biocontainment care units (BCU), which are specifically designed for the care of patients with highly contagious and hazardous diseases, such as COVID-19, Severe Acute Respiratory Syndrome (SARS), smallpox, and Ebola Virus disease. BCUs are typically grouped together and separated from normal patient care areas with secured entry and exit points, interlocking double-door access, and independent air-handling systems.
Advanced personal protective measures and procedures such as the use of personal protective equipment (PPE), cleaning and decontamination of units, waste disposal, and thorough and frequent hand hygiene are put in place in these units to ensure the safety of the healthcare workers and to contain the contamination and reduce the risk of cross-contamination.
The SimTigrate Design Lab at Georgia Institute of Technology (Atlanta) has been engaged in research on the design of biocontainment units from the perspective of both healthcare worker safety and the patient experience for several years. In September 2015, in the wake of the 2014 2014 West Africa Ebola outbreak, Georgia Tech, together with Emory University (Atlanta) and Georgia State University (Atlanta), initiated a multidisciplinary research program called “Prevention Epicenter of Emory and Atlanta Consortium Hospitals” and funded by the Centers for Disease Control and Prevention (CDC; Atlanta).
In this and several subsequent projects, the SimTigrate research team focused on the environmental design of the BCU and ways in which the built environment may support or hinder safe doffing of personal protective equipment (PPE).
Importance of safe donning and doffing areas
Highly infectious diseases can spread by airborne transmission (such as Rhinoviruses), through respiratory droplets being inhaled (such as SARS-CoV-2), or transmitted by direct contact with the body fluids of an infected person (such as Ebola Virus). Contact diseases also can spread by indirect contact with an infected person’s environment or personal items. For this reason, healthcare workers wear PPE that protects them from coming into contact with microbes during patient care.
Removal of PPE is recognized as a high-risk activity because the healthcare worker needs to extract themselves from the potentially contaminated PPE without it coming in contact with their bare skin. This is an especially difficult task following hours of direct patient care when staff are likely fatigued, contributing to errors and risky behaviors that can lead to potential acquisition of lethal pathogens.
Following the 2014 Ebola outbreak, the CDC updated its guidance on PPE, including specifying that donning and doffing areas need to be separated from the direct patient care area (patient room) and the layout should allow for a clear separation between clean and contaminated areas. Unidirectional throughput for staff and equipment should flow from clean to dirty and be clearly marked with visible signage (e.g., demarcation on the floor).
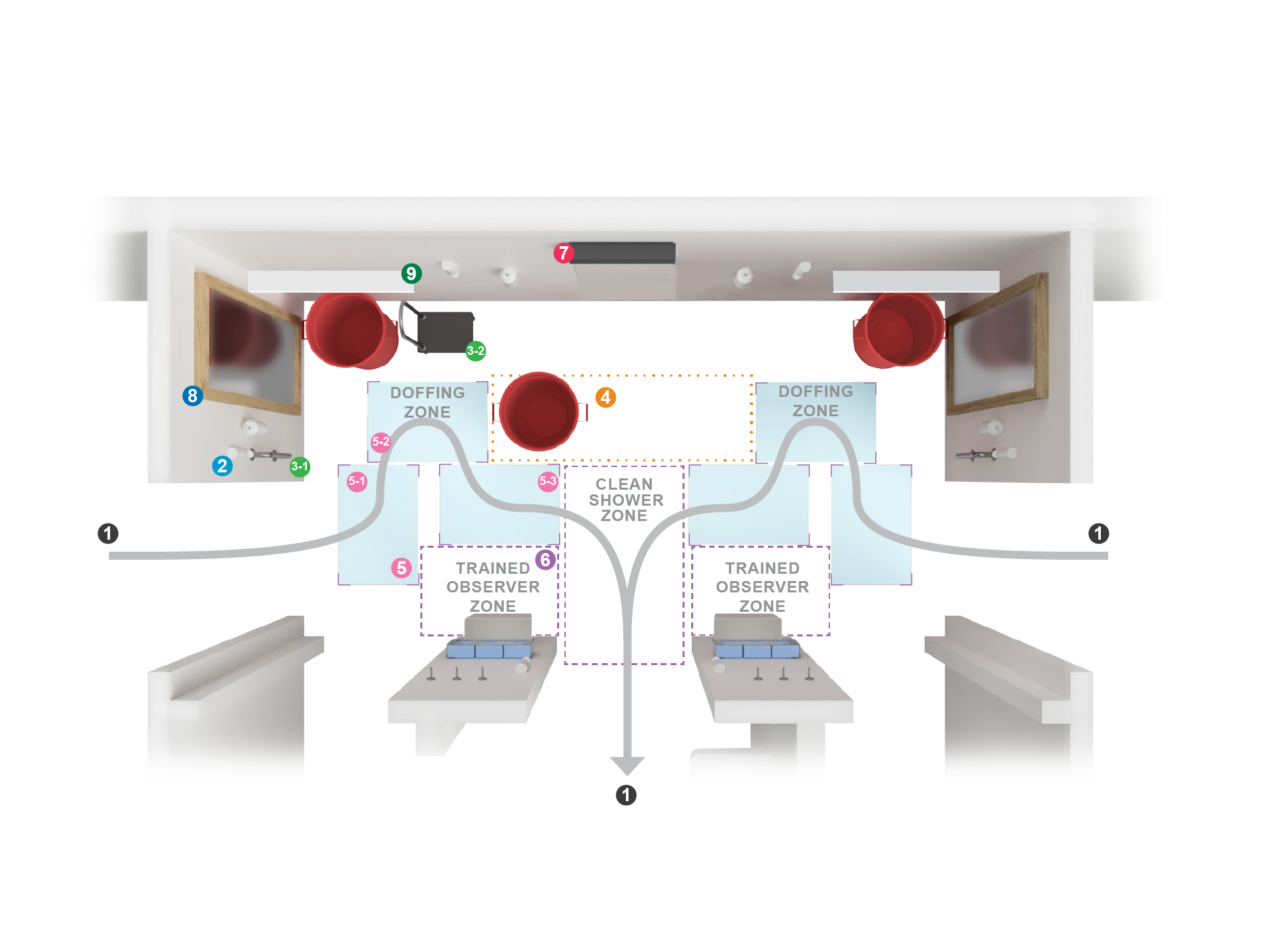
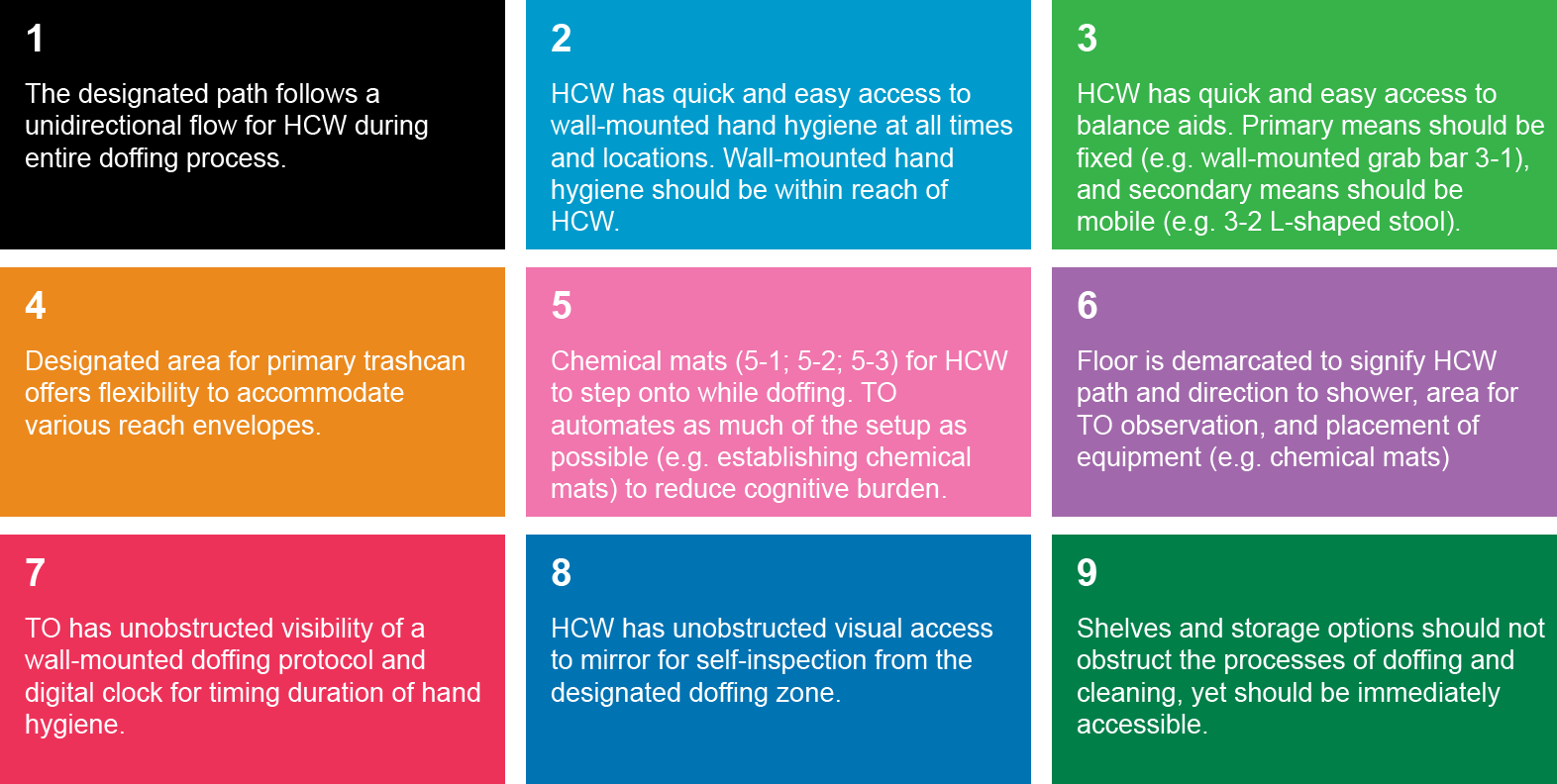
The doffing area should be large enough (approximately 80 square feet for a doffing area serving a single treatment room and 130 square feet if serving two patient rooms) to enable freedom of movement of staff during the process and to accommodate all the necessary equipment, such as a waste receptacle, alcohol-based hand rub dispensers, and clean glove supply. Additionally, all steps of PPE donning and especially doffing need to be visibly monitored by a trained observer (TO), who monitors compliance with all the protocols and assists the healthcare workers if needed.
Special design requirements for the doffing area
As part of the CDC-funded project, the SimTigrate Design Lab team observed 41 pairs of healthcare workers and trained observers during simulated doffing exercises in the four state-designated Ebola treatment centers in Georgia. The team identified 11 specific behaviors that healthcare workers performed, including stretching to reach a balance aid, moving the aid in the middle of the task or scooting, and touching the removed disposable shoe cover with both hands, that put staff at risk of occupational injury, contamination of the PPE, or contamination of the environment.
Researchers then sought environmental design strategies to discourage these behaviors. For example, floor demarcations helped guide and orient healthcare workers where to stand during doffing, and color-coded zones (red-hot, yellow-warm, green-cold) that indicated the risk of contamination made it easier for staff to follow a unidirectional flow. Floor demarcation also prevented staff from inadvertently leaving the doffing area and stepping back into the contaminated areas.
Furthermore, providing a built-in balance aid within reach reduced unstable postures and any inclination to move the aid while in the process of doffing, while placing a mirror directly in front of the healthcare worker allowed them to inspect their PPE without having to turn or bend.
As a result, the team identified five key requirements to support safe doffing of PPE: Facilitate communication between healthcare worker and trained observer; signify steps in the PPE doffing process; provide stabilization for the healthcare worker during PPE doffing; nudge/automate the safest choices; and promote situational awareness.
Later, the SimTigrate team tested a redesigned doffing area in a replicated, high-fidelity BCU mock-up that employed several of these strategies, with the results published in “Design strategies for biocontainment units to reduce risk during doffing of high-level personal protective equipment,” in the Journal of Clinical Infectious Diseases in September 2019. Among the findings, the study found that both the physical and cognitive load of healthcare workers, as well as the occurrence of risky behaviors, was significantly decreased, underscoring the role of the design of the doffing area as an important element of staff safety.
Optimized design for a dedicated biocontainment unit
Building on the knowledge gained through these studies, the SimTigrate Design Lab team was invited to help a large tertiary pediatric referral hospital in the Southeast optimize the design of a new 6-bed special care unit, which will treat children with highly infectious diseases such as SARS, smallpox, tularemia, plague, viral hemorrhagic fevers, and drug-resistant illnesses.
All key design decisions were developed in a codesign session with healthcare workers during simulation exercises at a full-scale, hospital mock-up. The research team observed interactions between staff and the built environment and together with healthcare workers reviewed the layouts, analyzed alternatives, and proposed specific design solutions to ensure the safety of the healthcare team.
The proposed biocontainment unit, which is planned to open in 2025, consists of two patient rooms connected by a large doffing area in the middle. Each patient room has an exterior window, a window to the doffing area, and a window to the corridor that allows for patient observation, staff communication, and communication between family members and the isolated patient.
The unit features unidirectional flow with a path that allows healthcare workers to move from clean to dirty areas without backtracking. Alternately, the middle zone can be modified to accommodate the doffing of two healthcare workers when both patient rooms are activated, with the doffing zone arranged with all the supplies and equipment duplicated and mirrored.
This optimized design of the doffing area supports better staff communication and efficiency and automates safer behavior by reducing the cognitive and physical load of healthcare workers and moving the cognition into the physical setting, making the safest behavior the easy choice.
Many of these environmental strategies can be achieved with little or no additional cost and easy-to-carry-out interventions, such as thoughtful placement of key items or demarcation of zones on floor to indicate risk of contamination. This can increase staff safety in biocontainment units and should be considered for implementation in both current and future biocontainment units, as well as when retrofitting non-traditional spaces like hotels or dormitories into alternate patient-care sites to address patient surge in a pandemic response.
Working together, researchers, designers, and clinicians can identify critical spatial requirements and problem areas. This approach can be applied to address other spaces where patients with serious communicable diseases are treated, as well as more routine patient care that needs to involve infection precautions in order to help deliver better patient care and keep healthcare providers safe.
Zorana Matić, M.Arch, is a researcher at the SimTigrate Design Lab (Atlanta) and a Ph.D. candidate at the School of Architecture, Georgia Institute of Technology. She can be reached at zorana.matic@gatech.edu. Benton Humphreys, B. Indd, is a graduate research assistant at the SimTigrate Design Lab and a candidate of the M.S. HCI program at Georgia Institute of Technology. He can be reached at benton.humphreys@gatech.edu. Jennifer DuBose, M.S., EDAC, is the associate director of the SimTigrate Design Lab and principal research associate in the College of Design at the Georgia Institute of Technology. She can be reached at jennifer.dubose@design.gatech.edu.
For more information on the SimTigrate Design Lab studies, visit http://bit.ly/2P64p4H and https://doi.org/10.1093/cid/ciz617.